Using Predictive Community Insights to Slow COVID-19 Hospitalizations
Just as national health officials warned ahead of the holiday season, the winter months of 2020-21 have proven to be the most challenging period of the COVID-19 pandemic so far. In Tennessee alone, there have […]
Just as national health officials warned ahead of the holiday season, the winter months of 2020-21 have proven to be the most challenging period of the COVID-19 pandemic so far. In Tennessee alone, there have been more than 10,000 deaths and nearly 18,000 hospitalizations resulting from SARS-CoV-2 infection. At distinct points over the last few months, hospitals have inched closer and closer to their breaking point. No community wants to be in the position of rationing care due to overwhelmed health systems. In January, LA County paramedics were instructed not to transport certain patients with a low chance of survival. Rising hospitalizations are a worrying indicator of this potential outcome in other cities.
How can local and state health officials and policymakers use their limited COVID-19 resources judiciously and in a targeted fashion to avoid these scenarios? With a slower than anticipated vaccine roll-out, delayed testing results, and more contagious variants of SARS-CoV-2 rapidly emerging, communities must be strategic in their efforts to combat the spread.
Predicting increased hospitalizations by community
Decode Health applies its predictive modeling approaches to identify rising COVID-19 hospitalizations at a population level across national, state, and local geographies. Over time, these models have been more than 85% accurate predicting the highest risk counties. Arming health officials and policymakers with this critical information – especially as they experience potential delays in receiving testing results – informs and supports rapid response needs for targeted testing, outreach and resource allocation in the communities most at risk.
Understanding the impact of demographic differences
Dramatic differences in COVID-19 outcomes can exist between demographic groups due to underlying social, environmental, and economic factors. According to data compiled by the APM Research Lab, Latinos are 2.5 times more likely to die of coronavirus than Whites in the U.S. The rate is 2.3 times for Black Americans.
The Center for Disaster Philanthropy points out, “What is common among these population groups is that racial discrimination has impacted their access to healthy food, safe and secure housing, good jobs and health care. This has resulted in increased instances of illnesses that align with the most dangerous co-morbidities associated with COVID-19 including diabetes, respiratory issues, heart issues, and high blood pressure. Suicide ideation [is also] higher among racialized groups.”
Decode Health uses collected data, local and regional public health information, and filtered, proprietary social determinants of health (SDOH) data to highlight specific locations and populations most at risk. This information helps stakeholders understand the social, physical, and environmental factors that contribute to distinct COVID-19 outcomes and develop targeted interventions to prevent hospitalizations.
Monitoring trends over time
Adding another layer of complexity, the relative importance of demographics can shift significantly over time. Since Decode Health has been analyzing Tennessee’s data since the start of the pandemic, we’ve been able to see how this can change, even week to week.
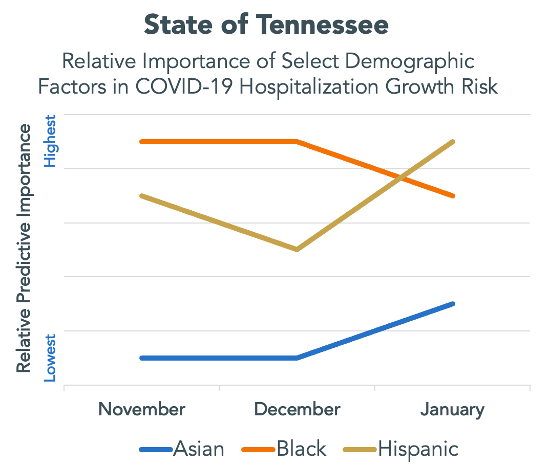
The chart below demonstrates trends across the State of Tennessee. African American predictive importance has slowly trended to be less important, while both Asian and Hispanic predictive importance has increased since December
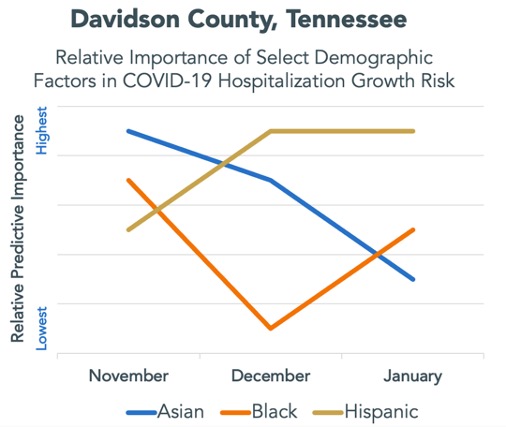
During the same period, here’s a look at Davidson County specifically where the City of Nashville is located. As you can see, it doesn’t always correspond to the same trends observed at the state level. This might be due to local mitigation and outreach efforts or better access to healthcare services. At Decode Health, we recognize that no two communities are exactly the same. This is why we continually collect information to understand the social, physical, and environmental factors that are present in the communities we serve. Analyzing the patterns of these unique characteristics alongside patient outcomes, such as hospitalizations that are a direct result of SARS-CoV-2 infection, allow us to understand the community risk factors that lead to better or worse patient outcomes. Having the ability to harness this information and focus our efforts on specific risk factors that lead to poor resilience to infection unlocks data-driven, proactive decision-making.
Leveraging the Decode Health Platform to Understand and Manage COVID-19 Hospitalizations
While new infection rates and hospitalizations are slowly trending downward according to recent forecasts from the Centers for Disease Control, we could see an increase in the coming weeks as novel coronavirus variants spread throughout the United States.
With the benefit of predictive data, how can resources be more strategically allocated to each demographic group? How might strategy be better at the state- and county-levels? Knowing where and when to deploy resources gives communities time to implement rational, targeted plans. Decode Health’s solution is easy to implement and flexible. With our advanced reporting and analytics capabilities, we can help health officials and policymakers make proactive decisions that make the best use of limited resources and ultimately save lives.